It is one of the most common treatable craniofacial pain syndromes.
It is a neuropathic syndrome characterized by episodes of severe agonizing facial pain originating from the trigeminal nerve, which supplies sensation to the face and mouth.
Although it can happen at any age, it is more commonly seen in people over the age of 50.
Structure of Trigeminal Nerve
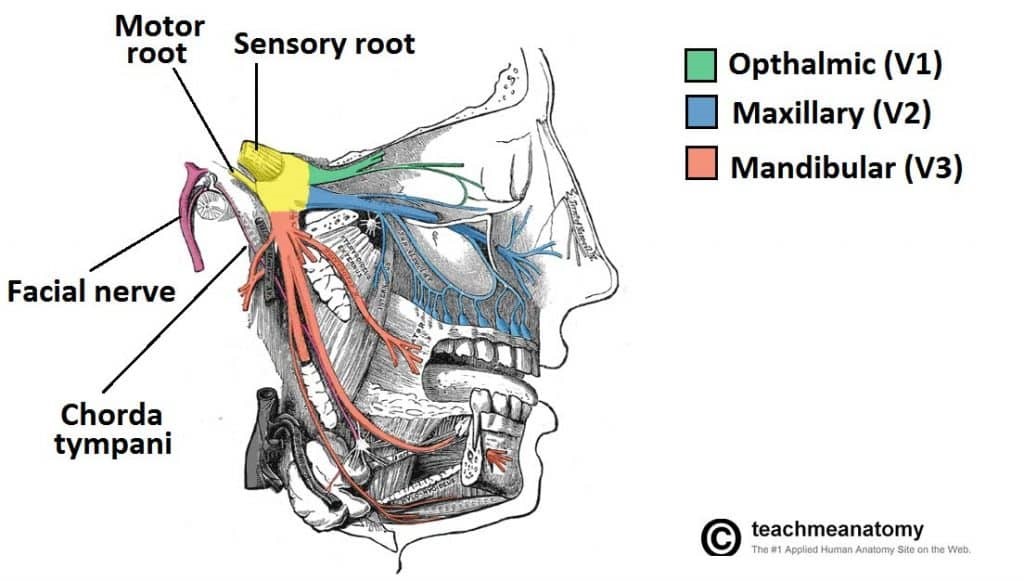
The trigeminal nerve has three major branches including the ophthalmic nerve (V1), maxillary nerve (V2) and the mandibular nerve (V3).
The ophthalmic (V1) division supplies sensation to the eye, forehead and bridge of the nose.
The maxillary (V2) division supplies sensory innervation to the upper lip, palate, upper teeth, gums, and the inner cheek below the eye.
The mandibular (V3) division provides sensation to the jaw, lower teeth, gums, lower lip, and side of the tongue.
The pain from trigeminal neuralgia may involve one, two or all three divisions of the trigeminal nerve, but most commonly involves the middle (Maxillary nerve V2) and lower (mandibular V3) branches.
Primary Trigeminal Neuralgia
Trigeminal neuralgia is caused by damage to the outer covering of the trigeminal nerve (the myelin sheath) leads to erratic and hyperactive transmission of nerve signals.
This can lead to attacks of pain caused by the misdirection of signals sub-serving normal painless sensation.
This type of damage to the nerve is usually the result of a small blood vessel along the surface of the nerve compresses the nerve as it enters the brainstem.
Most of the time such compression is caused by the superior cerebellar artery, but it can also be caused by other arteries and veins.
Secondary Trigeminal Neuralgia
Some patients will have a small tumor that compresses the nerve and causes the symptoms of trigeminal neuralgia.
A small fraction of patients with trigeminal neuralgia have multiple sclerosis which causes plaques within the nervous system.
Symptoms
The typical (type I) pain from trigeminal neuralgia is classically described as “stabbing,” or “electrical shock-like” in nature.
Episodes are typically sudden, brief bursts of facial pain often triggered by light touch around the mouth and face.
Sensory stimuli that often trigger the pain can include talking, brushing the teeth, eating, cold or a light breeze may trigger the pain.
The pain is usually a sharp electric like pain that can also occur spontaneously without a “trigger”.
The symptoms typically occur on one side of the face.
Patients can have periods of remission with pain-free intervals that last for minutes to weeks.
The attacks will often occur upon arising in the morning.
The atypical (type II) symptoms often include a more constant pain that is not triggered by touch and is associated with a more dull or burning sensation.
Diagnosis
Trigeminal neuralgia is diagnosed almost exclusively based on history, symptomatology and neurological examination.
Magnetic resonance imaging (MRI) scan performed to support the diagnosis and to exclude the possibility of a small tumor or multiple sclerosis.
Treatment Options
Medical treatment
The primary treatment of trigeminal neuralgia is pharmacological.
Mostly all of the doctors prefer to offer medical treatment for initial 4 to 5 years.
It is effective treatment where in medications are started with lowest effective dose and the gradually increased whenever low doses are found ineffective.
Surgical treatment
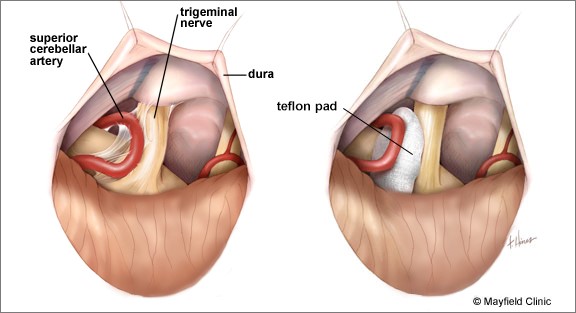
Microvascular decompression (MVD) is the most definitive and first-choice treatment option for patients that are fit to undergo general anesthesia.
The procedure offers the highest likelihood of long-term pain relief.
During a microvascular decompression a small opening is made into the skull behind the ear through the mastoid bone and the trigeminal nerve is directly inspected under an operating microscope.
Using microsurgical techniques, the surgeon identifies the offending vessel along the surface of the trigeminal nerve and a small piece of Teflon is inserted between the two to remove compression.
Most patients will have immediate pain relief after surgery and remain with substantially reduced or absent facial pain for years afterwards.
Other non-Invasive treatments
Stereotactic radiosurgery (CyberKnife or GammaKnife) is a painless non-invasive procedure where highly focused beams of radiation are accurately delivered to the root of trigeminal nerve.
It is performed on an outpatient basis and is a collaboration between the neurosurgeon and the radiation oncologist.
The pain relief with stereotactic radiosurgery generally occurs gradually over the period of few weeks.
This procedure is undertaken for elderly and medical unfit patients.
Other invasive treatments
Percutaneous glycerol rhizolysis is a minimally invasive procedure during which a small needle is inserted into the cheek and using x-ray guidance the needle is guided through a small skull foramen at the bottom.
The needle is advanced above into the foramen at the meckel’s cave, where the trigeminal ganglion is located.
Once the location of the needle is confirmed with contrast dye on x-ray, glycerol is injected into meckel’s cave and around the nerve.
The procedure is performed with light sedation and local anesthesia and most people are able to go home a few hours after the procedure.
Pain relief from glycerol rhizolysis is instantaneous.
There is often a small degree of facial numbness following the procedure that often subsides or becomes less after several weeks.
This is preferred in recurrence and patients who are medically unfit or elderly.